How NCInnovation Is Supporting Lifesaving Alzheimer’s Research
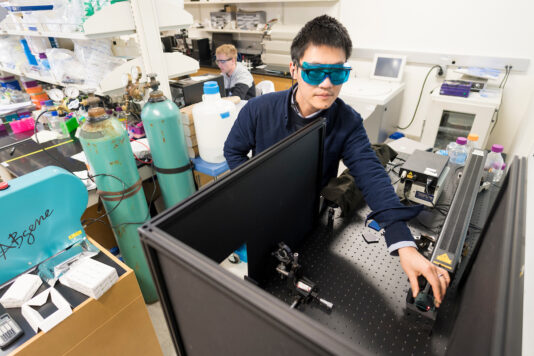
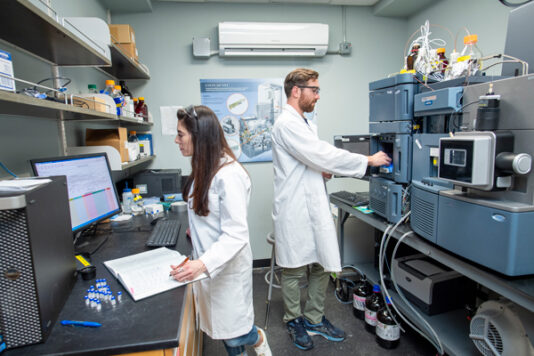
In a corner of the University of North Carolina at Pembroke campus, Dr. Ben Bahr leans over a microscope, studying neurons that hold the potential to rewrite the story of Alzheimer’s disease. Around him, undergraduate researchers move carefully through their lab routines, pipetting samples and recording data — part of a team chasing a simple but world-changing goal: help the brain regain the ability to clear disease-causing material..
Dr. Bahr, the William C. Friday Distinguished Professor of Molecular Biology and Biochemistry, has spent his career decoding how the brain clears out waste — and what happens when that system falters. “We’re conducting preclinical drug development to treat Alzheimer’s disease and other dementias, which together contribute to a global health crisis,” he said. “A drug to slow the disease progression and restore cognitive health could help millions maintain their memory, independence, and daily life.”
More than seven million Americans are living with Alzheimer’s — 50 million worldwide. For families in rural regions like those surrounding Pembroke, care access and early detection often lag behind major health systems. Bahr’s work, made possible through NCInnovation’s grant funding, aims to change that equation by developing a low-cost, easily administered oral therapy that targets the disease at its root cause.
Unlike existing FDA-approved antibody therapies that require expensive infusions and often carry serious side effects, Bahr’s approach enhances the brain’s own “cleaning crew” — the lysosomal pathway. This cellular machinery works like a recycling system, breaking down and removing misfolded, old, and/or toxic proteins that accumulate and disrupt memory and cognition. “By enhancing this pathway, we can increase the removal of multiple types of pathogenic material — not just one,” Bahr explained. “And our compound avoids the immune-related brain swelling that’s been a major issue with current therapies.”
Bahr’s lab has identified several series of small-molecule compounds, with patents, pending patents, and related supportive data that indicate a safe strategy to boost the clearance of multiple pathogenic proteins. The lead candidate drug has already passed initial safety tests and shows strong potential to slow — or even reverse — the damage to neuronal connections found in Alzheimer’s.
Central to the treatment strategy is a family of enzymes known as cathepsins, especially cathepsin B (also known as CatB). “CatB has a remarkable ability to degrade the toxic proteins including those that that form the hallmark aggregates found in Alzheimer’s disease” said Bahr. “Enhancing its activity reduces those aggregates and helps neurons recover their function.” His lab has shown that increasing CatB activity not only breaks down harmful proteins like Aβ42 but also restores resilience of neuronal connections and related learning ability. This fine-tuned biological approach could redefine how neurodegenerative diseases are is treated in the future.
While current approved drugs target a single pathogenic protein to treat Alzheimer’s disease, Bahr’s team is designing for the next frontier: enhancing clearance of multiple pathogenic proteins in the Alzheimer’s brain, to not only halt disease progression but also to prevent disease onset in those at risk of the disease. Human studies now make it possible to detect “proteinopathy” — the buildup of misfolded proteins — years and even decades before cognitive decline begins.
“Our goal is to intervene early, perhaps even in people in their 50s and 60s who show these early changes,” he said. Just as cholesterol-lowering medication helps prevent heart disease, this approach aims to treat protein buildup before memory loss begins.
This future — where a routine physical might include a simple brain-health test followed by an affordable oral medication — would not only change how the disease is managed but also who has access to treatment. Bahr notes that low-cost manufacturing routes mean his team’s compounds can be produced inexpensively and distributed widely, an advantage that could be especially meaningful for rural and underserved populations who too often go untreated.
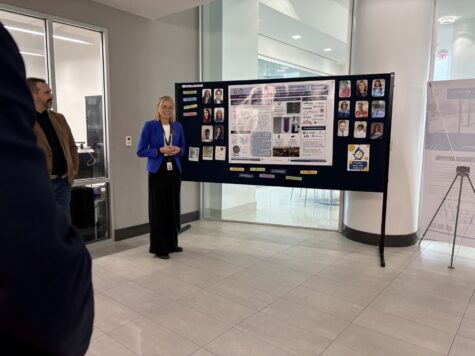
For years, Bahr’s groundbreaking research had been constrained by the limits of small-scale academic funding. “Such momentum didn’t happen until NCInnovation awarded the influential grant funding,” he said. The investment provided access to core facilities and collaborative networks across the UNC System — from Chapel Hill to UNC Wilmington and the Duke-UNC Alzheimer’s Disease Research Center — accelerating a pipeline of promising molecules toward clinical readiness.
Bahr credits NCInnovation with helping connect resources across institutions and enabling faster progress. The collaboration has already allowed his team to test compounds in human neurons and begin developing a regulatory roadmap — key steps toward eventual FDA approval.
Perhaps most inspiring is the way Bahr brings students into the work. His undergraduate researchers at UNCP gain experience typically reserved for graduate programs, contributing directly to experiments, data analysis, and even new molecular designs
Bahr envisions a future where Alzheimer’s and related dementias can be slowed, perhaps even prevented. The compounds his team has designed — rooted in decades of molecular insight and fueled by NCInnovation’s investment — may one day give millions of families more time, more memory, and more life.