Challenging the Assumption That Fibrosis Can’t Be Reversed
At the University of North Carolina at Chapel Hill, two scientists are challenging one of medicine’s most deeply rooted assumptions– that fibrosis is permanent and irreversible.
Dr. Ronit Freeman, a biomedical engineer, and Dr. James Hagood, a pediatric pulmonologist, arrived at the problem of fibrosis from very different disciplines. But both were driven by the same realization: something essential was missing from how the disease was being understood and treated.
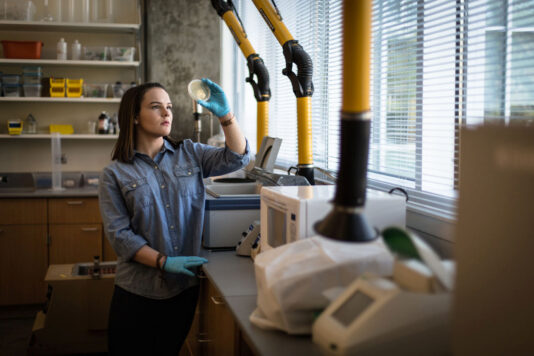
Freeman came to fibrosis research during her postdoctoral training, drawn to the microscopic environment that surrounds cells and quietly governs how they behave. “I was studying the environment that surrounds cells and how it guides both health and many different diseases,” she explained. As she dug deeper, it became clear that when that environment becomes imbalanced, it can drive devastating conditions like fibrosis. Rather than focusing only on downstream symptoms, Freeman began asking whether the environment itself could be re-engineered. “To better understand how an imbalance in that environment can cause illnesses like fibrosis, I decided to build a synthetic matrix to manipulate its parts and solve its problems,” she said. That decision would ultimately shape the direction of her career.
Hagood’s path was shaped at the bedside. As a physician, he was caring for children with pulmonary fibrosis and confronting the limits of available treatments firsthand. “I was seeing children with pulmonary fibrosis and realized treatments were ineffective, and the disease process was poorly understood,” he said. For patients and families, the options were grim. Current FDA-approved therapies can slow disease progression, but they do not cure fibrosis or reverse the damage already done. In many cases, patients face a prognosis of three to five years– or the possibility of a bilateral lung transplant.
That grim reality is one clinicians know all too well. Dr. Adam Goldstein, a family physician at UNC–Chapel Hill, has diagnosed and followed patients with pulmonary fibrosis for decades. He describes the disease as insidious– often emerging without a clear cause and progressing quietly until daily life becomes constrained by breathlessness, uncertainty, and fear. “Up until the last ten years, it was often fatal,” Goldstein said. “The inevitable slow but sure decline was difficult for patients, families, and providers.”
The collaboration between Freeman and Hagood began not through a grant or a formal initiative, but through what they now describe as a scientific “blind date,” arranged by a colleague who sensed a possible connection. At the time, each held a different piece of the puzzle. Freeman was engineering strategies to modulate the extracellular space that surrounds cells. Hagood was studying the biological effects of a key protein involved in fibrotic disease. When they began talking, the pieces clicked. What if fibrosis could be addressed from the outside in– not by simply slowing damage, but by activating the body’s own capacity to resolve it?
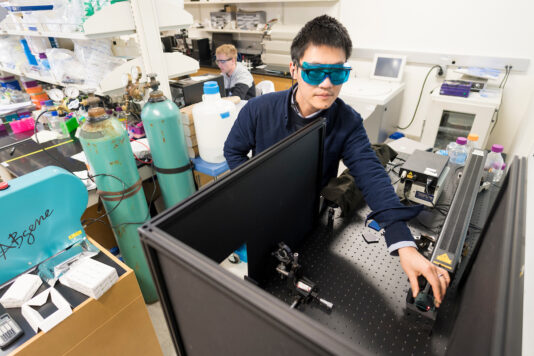
That question became the project’s “aha” moment. Together, Freeman and Hagood began imagining a weekly inhaled therapy designed not just to stall disease progression, but to initiate a fibrosis-resolving process. At the center of their approach is Thy-1, a naturally occurring protein known to reverse fibrosis. By understanding Thy-1’s critical molecular domains and targets, the team engineered a synthetic peptide that mimics its activity. Freeman describes the process as modular and precise– “like Lego pieces”– allowing the team to control how different parts of the protein come together in optimized ways. This ability to activate healing pathways while minimizing damaging ones represents a key scientific breakthrough in making fibrosis reversal conceivable.
From a clinician’s perspective, that distinction is profound. Goldstein notes that while today’s antifibrotic therapies can slow decline, they do not reverse scarring. Lung transplantation remains the only intervention proven to improve survival– and it is costly, limited by donor availability, and often not an option for older patients with other chronic conditions. What sets Freeman and Hagood’s work apart, he said, is its potential to go beyond slowing disease and toward actually reversing lung scarring– a shift that could fundamentally change care for patients and families.
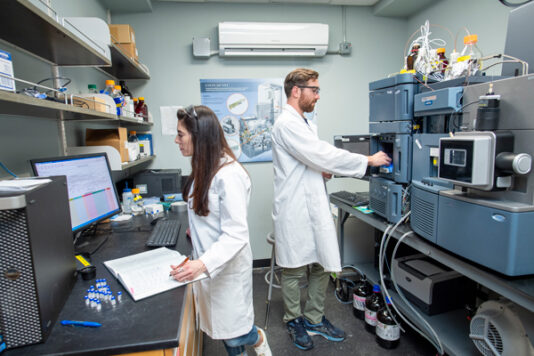
Turning that concept into something real has required an unusually tight convergence of disciplines. Freeman brings expertise in engineering and chemistry; Hagood contributes clinical insight and deep biological understanding. Around them is a broader interdisciplinary team of chemists, engineers, animal experimentalists, project managers, and business development experts. That convergence allows ideas to move more quickly from theory to testing.
Early commercial-stage support from the University of North Carolina at Chapel Hill also played a critical role in moving the work forward. Through UNC-Chapel Hill’s Office of Technology Commercialization and KickStart Venture Services—both part of the university’s Innovate Carolina initiative for innovation, entrepreneurship, and economic development—the team received guidance and resources to help translate early scientific discoveries toward real-world application.
One of the biggest challenges has been the lack of reliable animal models for lung fibrosis. To overcome this, the team developed methods using slices of human cadaver lungs, both healthy and fibrotic. Using advanced microscopy and image analysis, they test how their peptides affect real human tissue. For Freeman, seeing that restoration was a defining moment. “The first time we looked at lung tissues under the microscope that were previously highly fibrotic, and after treatment the fibrosis cleared, was a moment I will never forget,” she said.
For families living with fibrosis, those advances carry enormous emotional weight. Goldstein has experienced the disease not only as a physician, but personally. His father died from idiopathic pulmonary fibrosis in the 1990s after a prolonged decline. Years later, Goldstein recognized early symptoms in his brother-in-law, leading to a diagnosis and, ultimately, a life-saving double lung transplant at the start of the COVID-19 pandemic. Those experiences continue to shape how he evaluates emerging therapies—through the lens of what they could mean for real families over time.
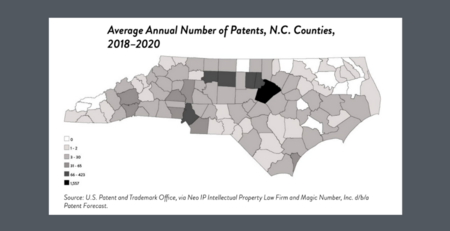
North Carolina has shaped both the urgency and the possibility of this work. The state has one of the highest incidence and mortality rates for pulmonary fibrosis in the nation, with related healthcare costs exceeding $2 billion annually. Risk factors such as COPD and burn pit exposure are prevalent, and North Carolina is home to one of the largest populations of veterans exposed to airborne hazards. At the same time, the state offers a dense ecosystem of research institutions, healthcare infrastructure, and pharmaceutical expertise.
Support from NCInnovation has been pivotal in bridging the gap between discovery and application. While traditional research grants often stop short of what is needed to move a technology toward the clinic, NCInnovation’s support has enabled critical screening and validation steps—advancing the team’s antifibrotic peptides to a higher level of readiness for clinical trials.
Looking ahead, success would mean more than a breakthrough drug. It would mean families no longer bracing for loss, physicians able to offer honest hope, and a healthcare system less defined by crisis and suffering. For Freeman and Hagood, that vision– and the patients behind it– remains the driving force.
“Science is often incremental,” Freeman reflected. “But when you’re working on a translational project like this, with the thought that something you’re doing could help someone live longer, breathe better, or play with their grandchild—we truly can’t think of anything more rewarding.”